
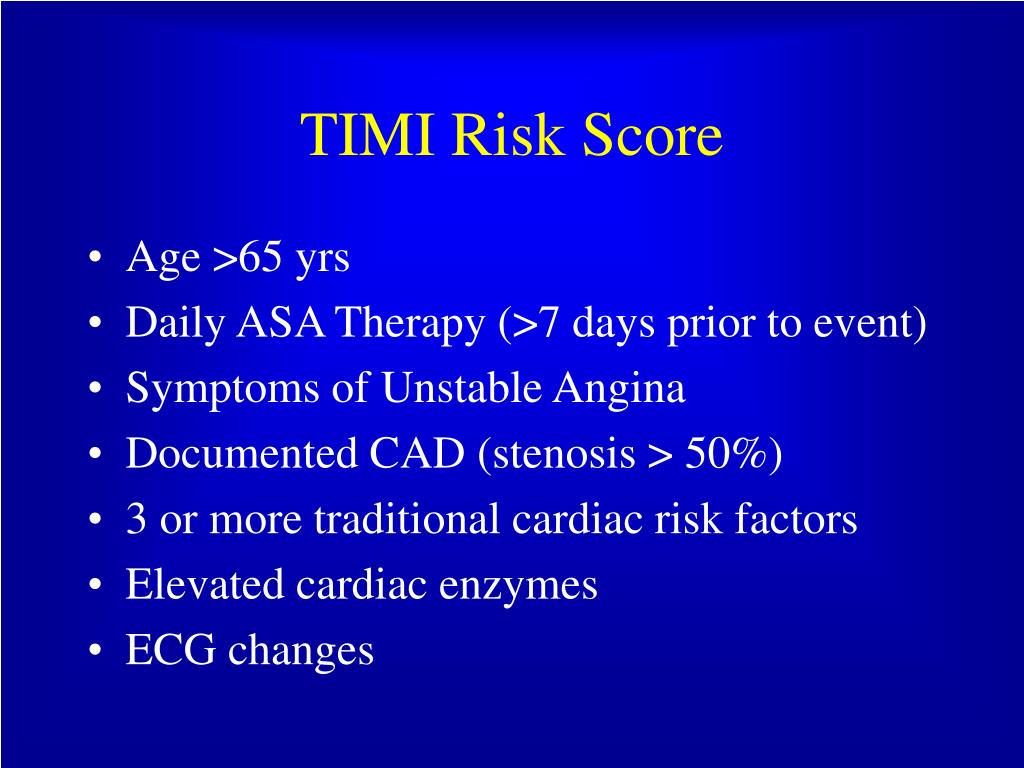
We used logistic regression model to derive a propensity score for early invasive strategy that included 63 variables. We performed a propensity score analysis to adjust for imbalances in baseline characteristics between early invasive group and late invasive group. A p less than 0.05 was deemed as significant. The 95 percent confidence interval for the relative risk was calculated with the use of the standard errors from the Kaplan-Meier curve. The relative risks were calculated by dividing the Kaplan-Meier estimated rate of an event in the early invasive strategy group by that of the late invasive strategy group. Categorical variables were compared with the use of the chi-square test, where appropriate. Continuous variables with normal distributions were expressed as mean ± SD and they were compared with the use of an unpaired Student's t-test. The statistical Package for Social Sciences (SPSS) for Windows, version 15.0 (Chicago, IL, USA) was used for all analyses. And the predictive factors for MACE at one-year clinical follow-up were calculated by multiple logistic regression analysis. The subgroup analysis was done according to each TIMI risk score and several baseline clinical features including age, gender, the presence or absence of diabetes mellitus, the presence or absence of ST-segment deviation, or the level of glomerular filtration rate. We compared the in-hospital mortality, the admission duration of coronary care unit, and the incidence of MACE during one-year clinical follow-up between two groups. All data were recorded on a standardized, electronic, web-based registry at. Re-infarction was defined as the recurrence of symptoms or electrocardiographic changes in association with a rise in cardiac enzymes above the normal upper limit. Major adverse cardiac events (MACE) at the six-month and one-year clinical follow-up were evaluated and were defined as the composite of 1) all cause death, 2) non-fatal MI, and 3) re-PCI or coronary artery bypass graft. Echocardiography was performed in all patients before discharge. And we calculated Thrombolysis In Myocardial Infarction (TIMI) risk score 11 of each patients at admission to Emergency Department. We analyzed baseline demographic and clinical characteristics, relevant laboratory results, and pharmacotherapy. Eligible patients for this study were required to have all three of the following: 1) symptoms of ischemia increasing or occurring at rest, 2) an elevated cardiac troponin I level (≥ 2.0 ng/mL) or CKMB (19 U/L, exceeding twice the upper limit of normal), and 3) ischemic changes assessed by electrocardiography, defined as ST-segment elevation, depression, or T-wave inversion of ≥ 0.2 mV in two contiguous leads. 2,845 patients (65.6 ± 12.5 years, 1,836 males) who were followed-up for one-year were included in the present study. 9, 10 Fifty high volume university, community centers with percutaneous coronary intervention (PCI) facilities and on-site cardiac surgery comprise the KAMIR. The KAMIR is a prospective, multi-center, observational registry designed to examine current epidemiology, inhospital management, and outcome of patients with acute MI in Korea for the commemoration of the 50th anniversary of the Korean Circulation Society. We compared two large patient cohorts obtained from the 50 multi-center KAMIR one consisting of consecutive acute myocardial infarction patients treated with early invasive strategy and the other patients treated with late invasive strategy. Therefore, we undertook the present study to analyze the clinical efficacy of the timing of revascularization and to test the hypothesis that an early invasive strategy is superior to a late invasive strategy for treating the NSTEMI patients who are registered in the Korea Acute Myocardial Infarction Registry (KAMIR). 5, 6 However, such recent advances in medical therapy as the early use of clopidogrel and intensive lipid-lowering therapy have been shown to improve the prognosis for patients suffering from acute coronary syndrome.
#Timi risk score early invasive trial
Recent Invasive versus Conservative Treatment in Unstable Coronary Syndromes (ICTUS) trial did not show superiority of an early invasive strategy for NSTEMI patients at the 1-year and 4-year clinical follow-up. 1 - 4 Despite these recommendations, it is not clear whether an early invasive strategy reduces mortality in non-ST-elevation myocardial infarction (NSTEMI) patients. The recent guidelines of the American College of Cardiology-American Heart Association (ACC/AHA) and the European Society of Cardiology (ESC) recommended an early invasive approach for the high-risk patients who suffer from acute coronary syndromes without ST-segment elevation.


 0 kommentar(er)
0 kommentar(er)
